
![]()
2020年11月接诊一例来自天津的17岁女性患儿(163cm,65kg),主诉:突发抽搐一次,排查时发现颅内占位1月余。患儿1个月前无明显诱因突发意识丧失伴四肢抽搐,持续时间不详,于当地医院发现颅内病变,遂来我院就诊。我院头颅CT/CTA示:左侧额叶异常高密度;左额动静脉畸形;头颅MRI示:左额叶异常血管影,动静脉畸形可能性大(28×24×37mm)。DSA示:畸形血管团,考虑动静脉畸形。
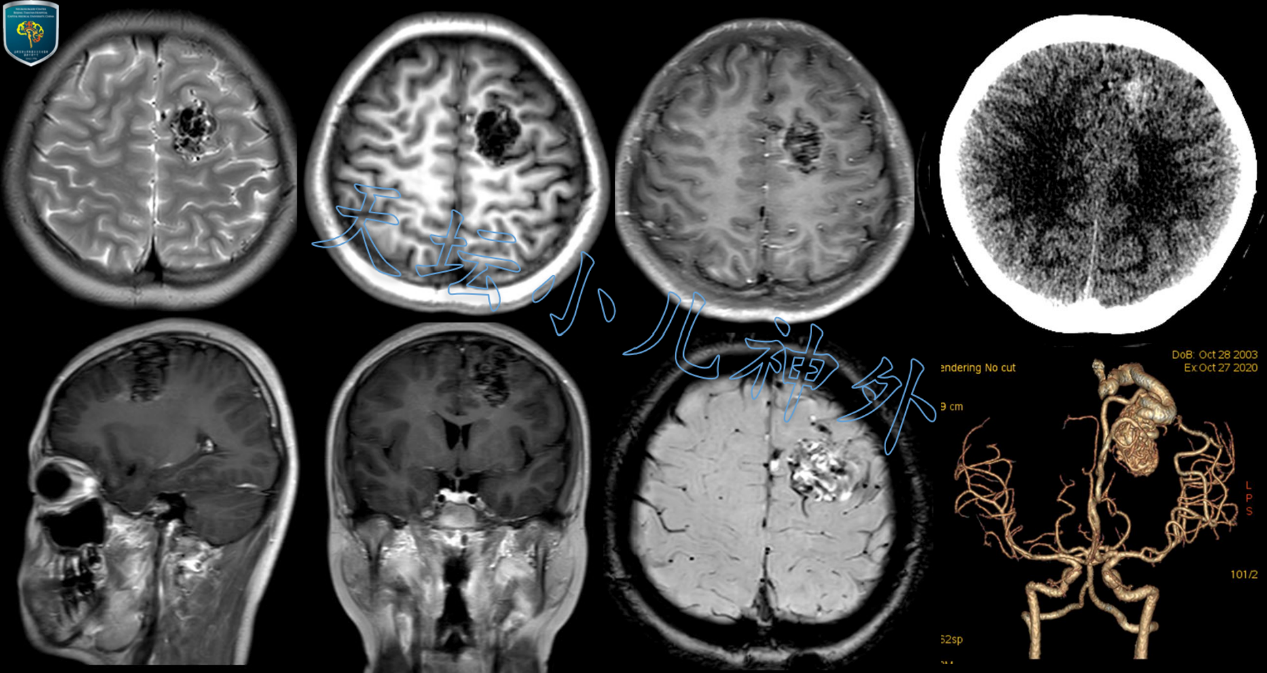
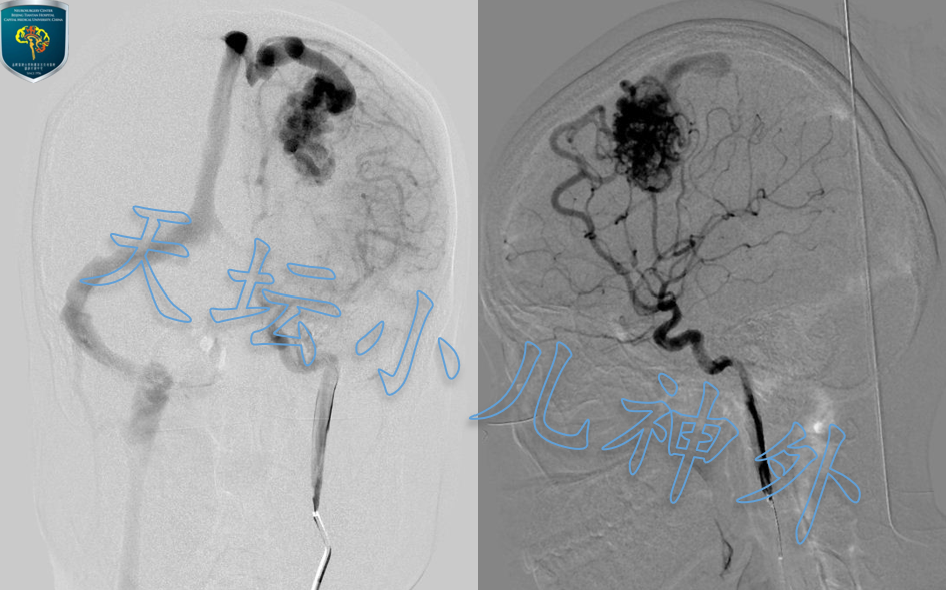
图1 CT:左侧额叶可见不规则团状迂曲稍高密度影;CTA:左额可见异常血管团,左侧ACA、MCA皮层支增粗参与供血,皮层见粗大引流血管汇入上矢状窦.MRI:左侧额叶见异常血管团,大小约28×24×37mm,SWI呈混杂信号,增强示病灶轻度强化.DSA:畸形血管团由左侧ACA、MCA参与供血,并见粗大的引流血管引流至上矢状窦.
患儿左额脑动静脉畸形诊断明确,合并症状型癫痫,具备手术指征,依据天坛医院小儿神外诊疗规范,患儿于2020年11月19日在神经导航引导下,行左侧额顶入路AVM切除术。剪开硬膜后,沿纵裂探查左侧额叶,见畸形血管团,色红、团块蚯蚓状,范围约2×3×4cm,中线处可见一支粗大引流静脉汇入上矢状窦,导航精确划定病变范围,依次游离畸形血管团前界、外侧、后界,见两支分别来源于左侧大脑前动脉、左侧大脑中动脉的粗大供血动脉,蛇牌720动脉瘤夹两枚予以夹闭后电凝切断,畸形血管团质地明显变软并缩小,继而游离中线处,电凝切断粗大引流静脉,畸形血管团完整切除。手术顺利,术中出血100ml,未输血。
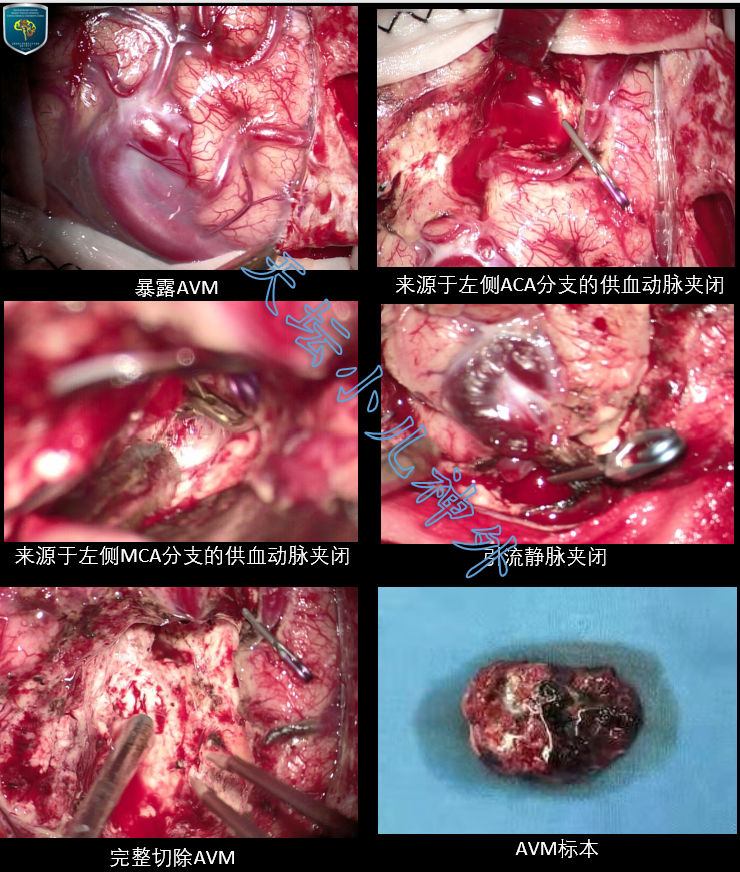
图2 术中所见及标本照片.
术后患儿恢复良好,无新增神经系统阳性体征,术后复查头颅CT/CTA/MRI/DSA显示畸形血管团完整切除。病理回报示:动静脉畸形.术后10天顺利出院,随访中。
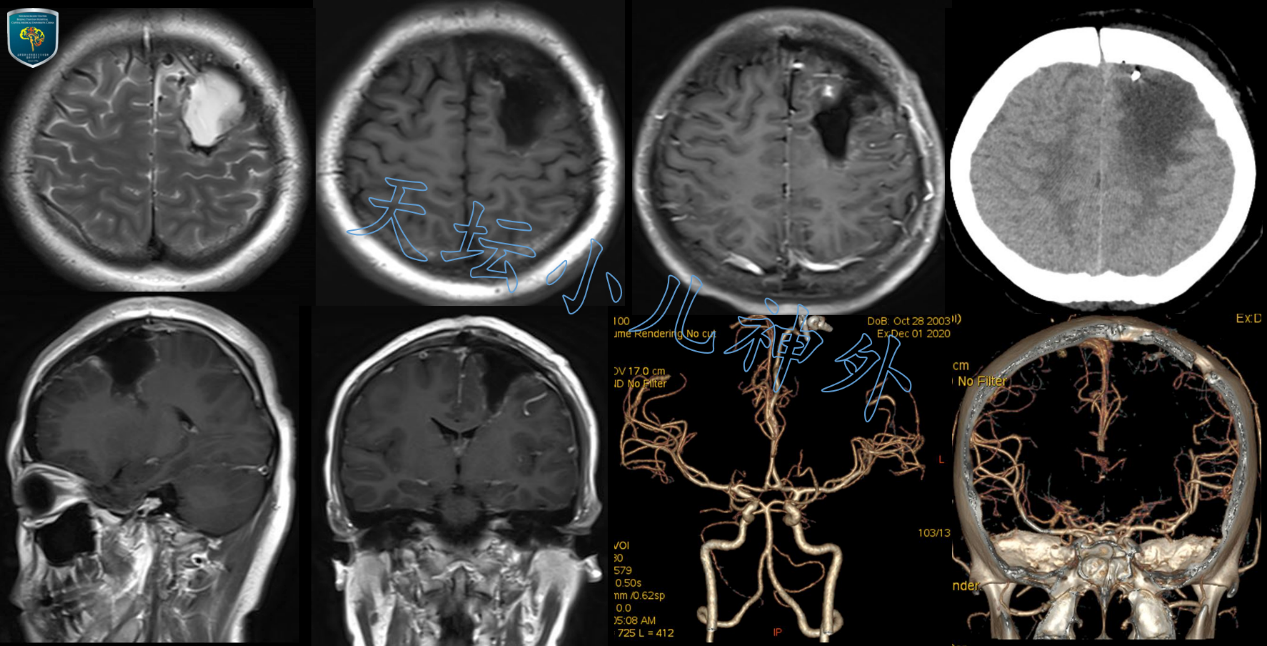
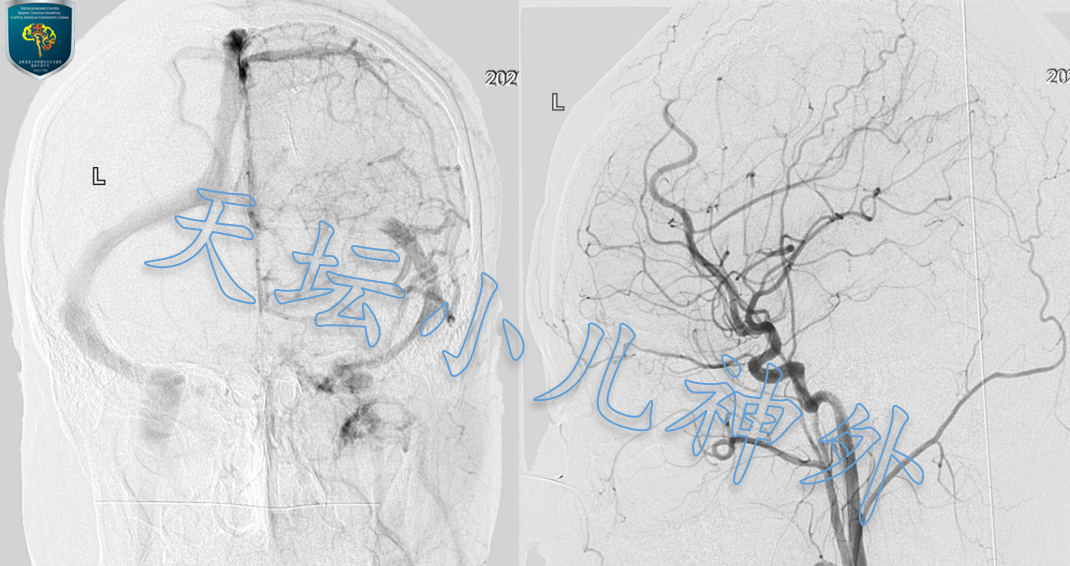
图3 术后CT/CTA/MRI/DSA显示:左额动静脉畸形血管团完整切除.
治疗体会
颅内动静脉畸形(arteriovenous malformations,AVM)是常见颅内血管性疾病,本质上是一团发育不良的血管,其供血动脉与引流静脉直接相连,之间无正常毛细血管床,形成高流量、低阻力的瘘管,将血液从动脉直接分流到静脉系统1。人群发病率约为50/10万2,发病年龄多在20-40岁3,儿童患者仅占发病人群的15%4。约半数患者合并颅内出血,20%-25%的患者可表现为局灶或全面性癫痫发作,15%的患者合并头痛、认知功能障碍,甚至无任何症状5-9。
我们认为,手术切除畸形血管团是治疗AVM的首选方案,一旦手术完整切除,患儿可以终身治愈。澳大利亚高级医学院的David Bervini等人在2014年的一组单中心427例未出血颅内AVM手术研究中曾报道,Spetzler–Martin分级在I-II级的患者术后出现严重并发症仅为2%10;美国波士顿儿童医院和犹他儿童医院在对97名AVM患儿术后中位随访时间65个月的研究中发现,Spetzler–Martin分级为I、II级的患儿分别有82.8%和63.9%术后未出现神经功能缺失,且所有患儿中,85.5%术后可独立生活11;加利福尼亚大学脑血管病研究中心的一项232例报道Spetzler–Martin分级I-II级患者手术死亡率为0%12。可见,针对颅内AVM,尤其是属于Spetzler–Martin分级I-II级患者,应积极手术予以根治,效果良好。
至于血管介入栓塞治疗,通常用于术前缩小AVM体积、术中降低出血风险。若以治疗为目的单纯血管内栓塞,治愈率仅为51%13-15,栓塞术中出血风险高达7%16,故一般不建议单独应用栓塞治疗AVM。
关于立体定向放射治疗(伽玛刀),优势在于一旦成功,便可以最小的风险获得最大的收益17-23,但问题有二:第一,放疗完成后,血管不会立即闭塞,而是需要一段潜伏期才能闭塞至最大程度,最长可达4年;第二,放疗会导致毗邻正常脑组织放射性损伤1。一组多中心1051例AVM患者的回顾分析中,放疗后治愈率为75.2%,出血率7.2%,其它并发症发生率6.5%,死亡率1.2%12。治疗效果优于单纯血管内介入栓塞,不及手术治疗。
本例患儿病变位于非功能区、团块样较局限,供血动脉明确,引流静脉较表浅,Spezler-Martin分级为II级,首选开颅手术治疗。Lawton等人认为1,AVM切除术的关键点有两个:一是引流静脉最后切断;二是尽可能靠近畸形血管团切除病变,保护毗邻脑组织。因此,应用术中神经导航,精准定位病灶范围,引导切除供血动脉及引流静脉,就显得尤其重要。
参考文献
1. Lawton,M. T. et al. Brain arteriovenous malformations. Nat Rev DisPrimers 1, 15008, doi:10.1038/nrdp.2015.8 (2015).
2. Morris,Z. et al. Incidental findings on brain magnetic resonanceimaging: systematic review and meta-analysis. BMJ (Clinicalresearch ed.) 339, b3016, doi:10.1136/bmj.b3016 (2009).
3. Hofmeister,C. et al. Demographic, morphological, and clinicalcharacteristics of 1289 patients with brain arteriovenousmalformation. Stroke 31, 1307-1310,doi:10.1161/01.str.31.6.1307 (2000).
4. Jimenez,J. E. et al. Role of follow-up imaging after resection ofbrain arteriovenous malformations in pediatric patients: a systematicreview of the literature. Journal of Neurosurgery: Pediatrics19, 149-156, doi:10.3171/2016.9.Peds16235 (2017).
5. Fults,D. & Kelly, D. L., Jr. Natural history of arteriovenousmalformations of the brain: a clinical study. Neurosurgery 15,658-662, doi:10.1227/00006123-198411000-00003 (1984).
6. Crawford,P. M., West, C. R., Chadwick, D. W. & Shaw, M. D. Arteriovenousmalformations of the brain: natural history in unoperated patients.Journal of neurology, neurosurgery, and psychiatry 49,1-10, doi:10.1136/jnnp.49.1.1 (1986).
7. Ondra,S. L., Troupp, H., George, E. D. & Schwab, K. The natural historyof symptomatic arteriovenous malformations of the brain: a 24-yearfollow-up assessment. Journal of neurosurgery 73,387-391, doi:10.3171/jns.1990.73.3.0387 (1990).
8. ApSimon,H. T., Reef, H., Phadke, R. V. & Popovic, E. A. Apopulation-based study of brain arteriovenous malformation: long-termtreatment outcomes. Stroke 33, 2794-2800,doi:10.1161/01.str.0000043674.99741.9b (2002).
9. Englot,D. J. et al. Seizure predictors and control aftermicrosurgical resection of supratentorial arteriovenous malformationsin 440 patients. Neurosurgery 71, 572-580; discussion580, doi:10.1227/NEU.0b013e31825ea3ba (2012).
10. Bervini,D., Morgan, M. K., Ritson, E. A. & Heller, G. Surgery forunruptured arteriovenous malformations of the brain is better thanconservative management for selected cases: a prospective cohortstudy. Journal of neurosurgery 121, 878-890,doi:10.3171/2014.7.Jns132691 (2014).
11. Ravindra,V. M. et al. A study of pediatric cerebral arteriovenousmalformations: clinical presentation, radiological features, andlong-term functional and educational outcomes with predictors ofsustained neurological deficits. Journal of Neurosurgery:Pediatrics 24, 1-8, doi:10.3171/2019.2.Peds18731 (2019).
12. Potts,M. B. et al. Current surgical results with low-grade brainarteriovenous malformations. Journal of neurosurgery 122,912-920, doi:10.3171/2014.12.Jns14938 (2015).
13. Saatci,I., Geyik, S., Yavuz, K. & Cekirge, H. S. Endovascular treatmentof brain arteriovenous malformations with prolonged intranidal Onyxinjection technique: long-term results in 350 consecutive patientswith completed endovascular treatment course. Journal ofneurosurgery 115, 78-88, doi:10.3171/2011.2.Jns09830(2011).
14. Pierot,L. et al. Endovascular treatment of brain arteriovenousmalformations using a liquid embolic agent: results of a prospective,multicentre study (BRAVO). European radiology 23,2838-2845, doi:10.1007/s00330-013-2870-6 (2013).
15. Baharvahdat,H. et al. Hemorrhagic complications after endovasculartreatment of cerebral arteriovenous malformations. AJNR. Americanjournal of neuroradiology 35, 978-983,doi:10.3174/ajnr.A3906 (2014).
16. Kato,Y. et al. Expert Consensus on the Management of BrainArteriovenous Malformations. Asian J Neurosurg 14,1074-1081, doi:10.4103/ajns.AJNS_234_19 (2019).
17. Kemeny,A. A., Dias, P. S. & Forster, D. M. Results of stereotacticradiosurgery of arteriovenous malformations: an analysis of 52 cases.Journal of neurology, neurosurgery, and psychiatry 52,554-558, doi:10.1136/jnnp.52.5.554 (1989).
18. Lunsford,L. D. et al. Stereotactic radiosurgery for arteriovenousmalformations of the brain. Journal of neurosurgery 75,512-524, doi:10.3171/jns.1991.75.4.0512 (1991).
19. Dwenger,A., Funck, M., Lueken, B., Schweitzer, G. & Lehmann, U. Effect ofascorbic acid on neutrophil functions and hypoxanthine/xanthineoxidase-generated, oxygen-derived radicals. European journal ofclinical chemistry and clinical biochemistry : journal of the Forumof European Clinical Chemistry Societies 30, 187-191,doi:10.1515/cclm.1992.30.4.187 (1992).
20. Steiner,L. et al. Clinical outcome of radiosurgery for cerebralarteriovenous malformations. Journal of neurosurgery 77,1-8, doi:10.3171/jns.1992.77.1.0001 (1992).
21. Yamamoto,M. et al. Long-term follow-up of radiosurgically treatedarteriovenous malformations in children: report of nine cases.Surgical neurology 38, 95-100,doi:10.1016/0090-3019(92)90084-z (1992).
22. Yamamoto,M., Jimbo, M., Hara, M., Saito, I. & Mori, K. Gamma kniferadiosurgery for arteriovenous malformations: long-term follow-upresults focusing on complications occurring more than 5 years afterirradiation. Neurosurgery 38, 906-914,doi:10.1097/00006123-199605000-00010 (1996).
23. Karlsson,B., Lindquist, C. & Steiner, L. Prediction of obliteration aftergamma knife surgery for cerebral arteriovenous malformations.Neurosurgery 40, 425-430; discussion 430-421,doi:10.1097/00006123-199703000-00001 (1997).







