2020年10月接诊一例来自山西的7岁男性患儿(130cm,28kg),主诉为“后枕、颈、肩部阵发性疼痛2年,进行性加重”。疼痛发作时,头颈部针刺样刺痛,每次持续约10分钟后自行缓解。查体示:患儿神清语利、自主体位,肌力肌张力正常,无感觉分离障碍,无双手鱼际肌萎缩。我院3D-CT除外扁平颅底及颅底凹陷(图1);MRI提示:小脑扁桃体下疝并C2脊髓空洞形成(图2)。
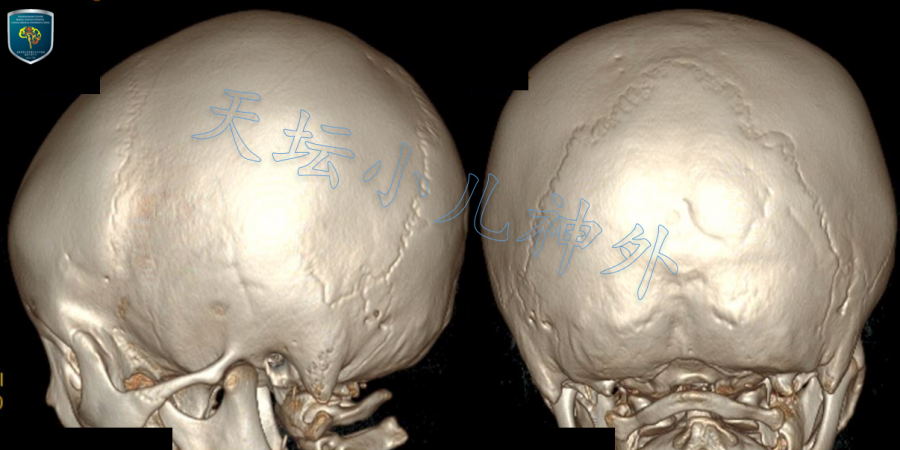
图1.术前CT未见明显扁平颅底及颅底凹陷。
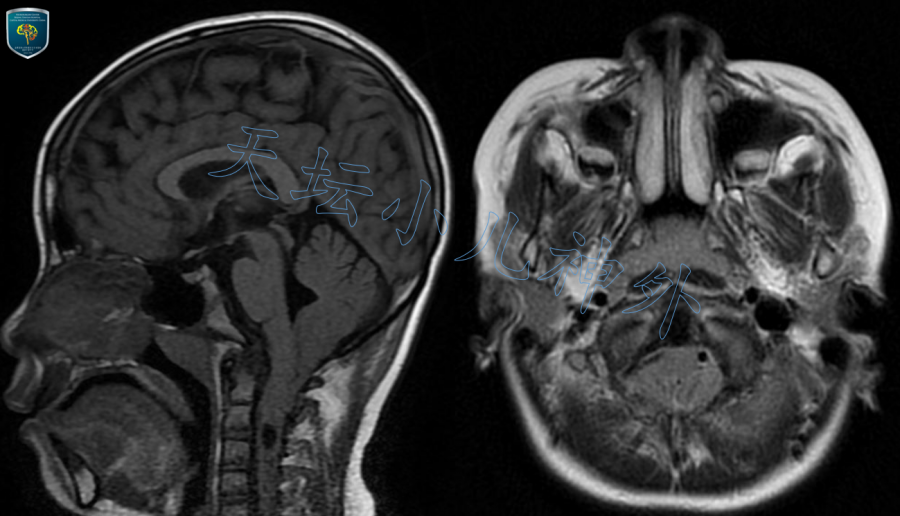
图2.术前MR显示典型Chiari畸形 I型表现。
鉴于患儿有特征性头颈肩部疼痛,影像学呈典型Chiari畸形 I型表现,小脑扁桃体下疝超过5mm,合并脊髓空洞,具备手术指征。依据天坛小儿神外诊疗规范,于2020-10-08在全麻下行“后正中入路枕下减压+扁桃体还纳+硬膜扩张成形术”。患者左侧卧位,头架固定,枕下后正中切口,取自体筋膜4X3cm备用。沿中线分离,撑开两侧肌肉暴露骨板,枕骨近枕大孔处骨质明显增厚内陷,咬除该部分骨质,范围约4X3cm;继而咬除寰椎后弓,见寰枕筋膜明显增厚,予以剔除;于寰枕交界处“Y”型剪开增厚的硬膜,见双侧小脑扁桃体挤压变形,疝入椎管(图3)。剔除蛛网膜,低功率双极电灼扁桃体下极,至双侧扁桃体挛缩上抬,还纳入颅,枕大池脑脊液涌出,寰枕交界处充分减压,小脑后下动脉及穿支血管保护完好,术区彻底止血,冲洗清亮。最后采用自体筋膜减张严密缝合硬脑膜(图4)。
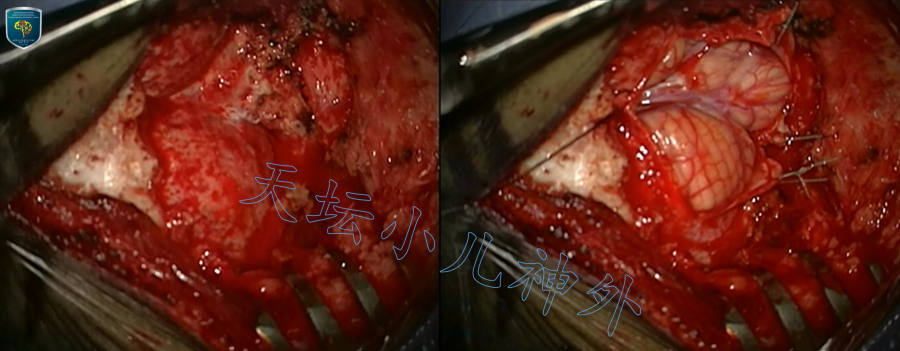
图3.枕下减压,骨窗大小4X3cm,寰枕筋膜及寰枕部硬膜明显增厚,双侧小脑扁桃体受挤压变形,疝入椎管。
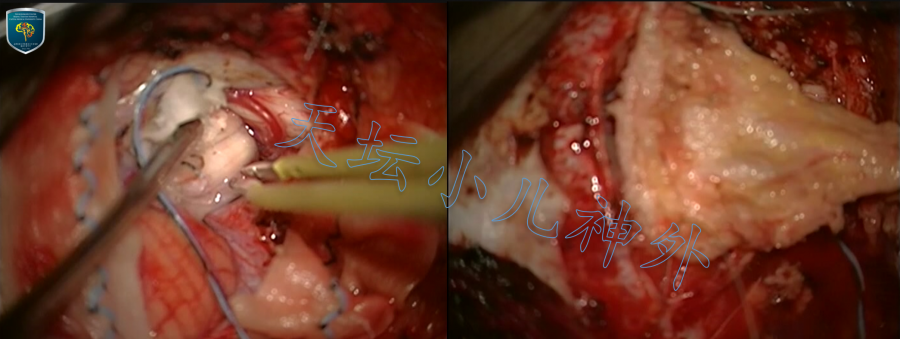
图4.低功率双极电灼双侧扁桃体,使之挛缩上抬,还纳入颅。寰枕交界处充分减压,脑脊液流出通畅(左图);寰枕交界充分减压后,自体筋膜减张严密缝合。(右图)
术后患者一般情况好,头颈疼痛缓解明显。术后当晚颅脑CT显示枕下减压充分(图5);术后1周复查头颈MR提示脊髓空洞较前明显缩小,寰枕交界处不再拥挤。患儿术后恢复好,颈托保护,无神经系统功能缺失,术后十天顺利出院。术后1月来院复查,头颈疼痛消失,头颈MR提示小脑扁桃体还纳满意,颈髓空洞消失(图6、7)。
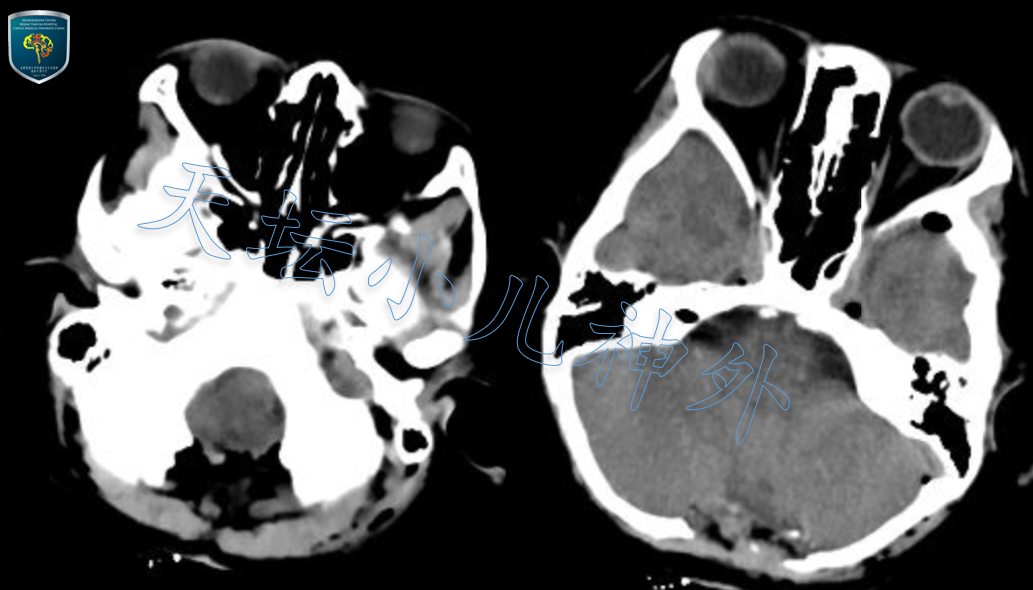
图5.术后当晚复查头颅CT显示枕下减压满意。
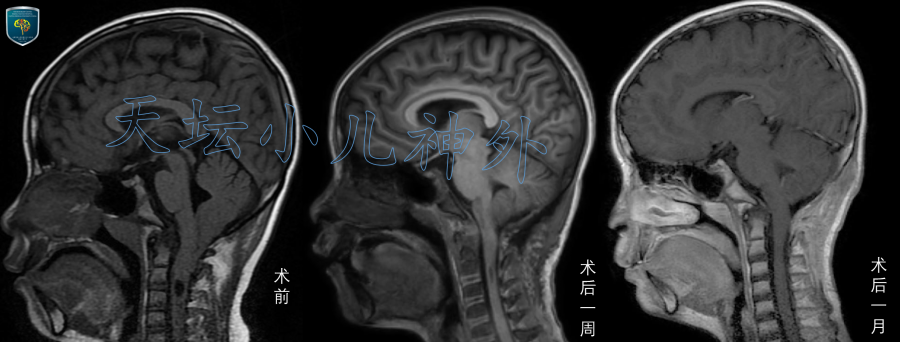
图6:术后1周(图中)及1月(图右)复查头颈MR,提示小脑扁桃体还纳入颅,脊髓空洞消失。
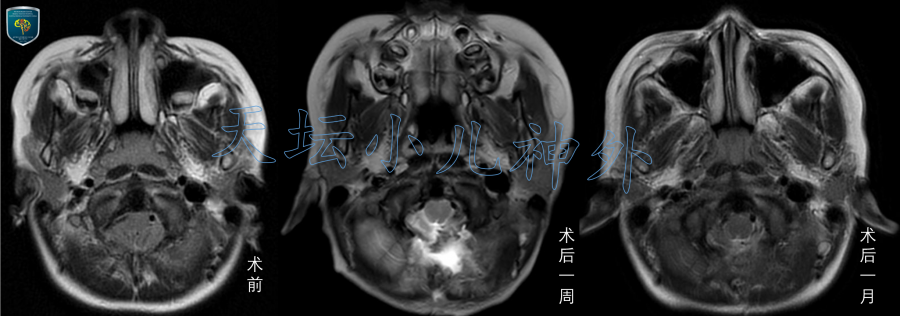
图7. 术后1周(图中)及1月(图右)复查头颈MR,提示小脑扁桃体还纳满意。
治 疗 体 会:
Chiari畸形的诊断标准是小脑扁桃体疝出部分超出McRae线(枕大孔前后连线)5mm1。临床上Chiari I型最为常见,如本例,形成机理可能是先天性后颅窝容积发育不充分,脑内容物相对拥挤而疝出颅腔。Chiari I型在普通人群中的发生率高达0.5-3.6%,好发于0-10岁儿童2-4,多数不需手术治疗。什么情况下需要手术,国内外并没有公认的标准。依据天坛小儿神外的经验,如果出现下述情况:1.小脑扁桃体下疝大于5mm;2.有明确的临床症状,常见者如头颈交界部疼痛,屏气、提重物时(Valsalva动作)可加重;3.有明确的症状体征,如鱼际肌萎缩、深浅感觉分离等;4.合并脊髓空洞。患儿在第1条的基础上,合并2,3, 4任意一条,即建议手术。
儿童Chiari I型并无统一术式,国内外曾采用过单纯枕下骨减压5、骨减压+硬膜外层松解术6、小脑扁桃体切除术7、小脑扁桃体电凝术8、寰枢椎融合术9等方法。北京天坛医院小儿神外采用枕下骨减压+扁桃体还纳+硬膜扩张成形术。该术式安全、便捷,减压充分,并发症少,患儿临床症状明显缓解,值得推广。
参考文献:
1. Barkovich AJ, Wippold FJ, Sherman JL, Citrin CM. Significance of cerebellar tonsillar position on MR. AJNR American journal of neuroradiology. 1986;7(5):795-799.
2. Chatrath A, Marino A, Taylor D, Elsarrag M, Soldozy S, Jane JA, Jr. Chiari I malformation in children-the natural history. Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2019;35(10):1793-1799.
3. Smith BW, Strahle J, Bapuraj JR, Muraszko KM, Garton HJ, Maher CO. Distribution of cerebellar tonsil position: implications for understanding Chiari malformation. Journal of neurosurgery. 2013;119(3):812-819.
4. Strahle J, Muraszko KM, Kapurch J, Bapuraj JR, Garton HJ, Maher CO. Chiari malformation Type I and syrinx in children undergoing magnetic resonance imaging. Journal of neurosurgery Pediatrics. 2011;8(2):205-213.
5. Mortazavi MM, Tubbs RS, Hankinson TC, Pugh JA, Cohen-Gadol AA, Oakes WJ. The first posterior fossa decompression for Chiari malformation: the contributions of Cornelis Joachimus van Houweninge Graftdijk and a review of the infancy of "Chiari decompression". Child's nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2011;27(11):1851-1856.
6. Lu VM, Phan K, Crowley SP, Daniels DJ. The addition of duraplasty to posterior fossa decompression in the surgical treatment of pediatric Chiari malformation Type I: a systematic review and meta-analysis of surgical and performance outcomes. Journal of neurosurgery Pediatrics. 2017;20(5):439-449.
7. Gardner WJ, Angel J. The mechanism of syringomyelia and its surgical correction. Clinical neurosurgery. 1958;6:131-140.
8. Villa A, Imperato A, Maugeri R, Visocchi M, Iacopino DG, Francaviglia N. Surgical Treatment in Symptomatic Chiari Malformation Type I: A Series of 25 Adult Patients Treated with Cerebellar Tonsil Shrinkage. Acta neurochirurgica Supplement. 2019;125:125-131.
9. Goel A. Is atlantoaxial instability the cause of Chiari malformation? Outcome analysis of 65 patients treated by atlantoaxial fixation. Journal of neurosurgery Spine. 2015;22(2):116-127.